Leprosy (Hansen's disease)
Leprosy is a chronic infectious disease caused by a bacteria called Mycobacterium leprae, or M. leprae. The bacteria primarily infect the skin and nerves. It is curable with antibiotics, but if not treated, it can cause blindess, disfigurement, and severe disabilities.
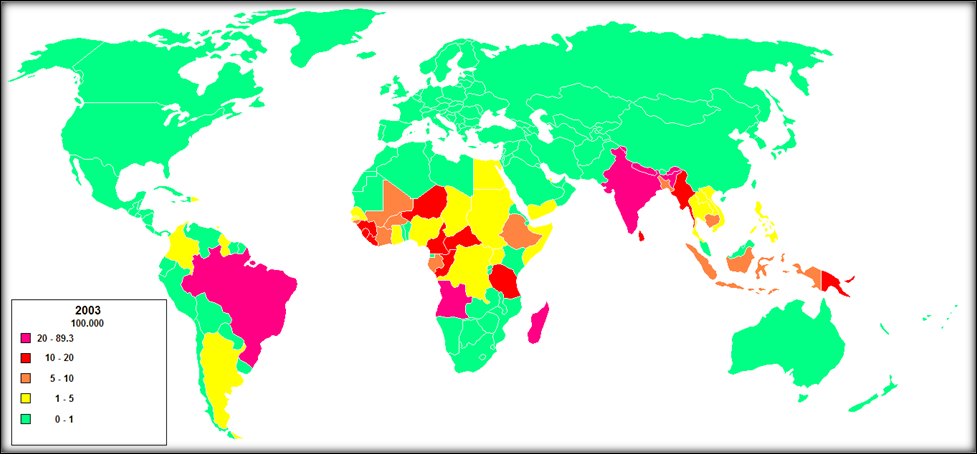
Leprosy has been known since ancient times, with the earliest currently known case having occurred 4,000 - 4,500 years ago in India (1). It is believed to have spread from India or eastern Africa, arriving in Europe during or after the 4th century B.C.E. (2, 3). It was endemic in Europe and other cooler climates in the past, but today, it tends to occur in warm parts of the world (see map below).
Leprosy has long carried a powerful social stigma. In past centuries, patients were made to live outside of the general community. In Europe, they were forced to carry bells or clappers to announce their presence, so that others could hide from them (see painting below). Today, it is known that roughly 95% of the population is not susceptible to infection with M. leprae. In addition, antibiotics are very effective treating leprosy. Most importantly, patients are no longer infectious after taking only a few doses of medicine. For more information see reference 4.
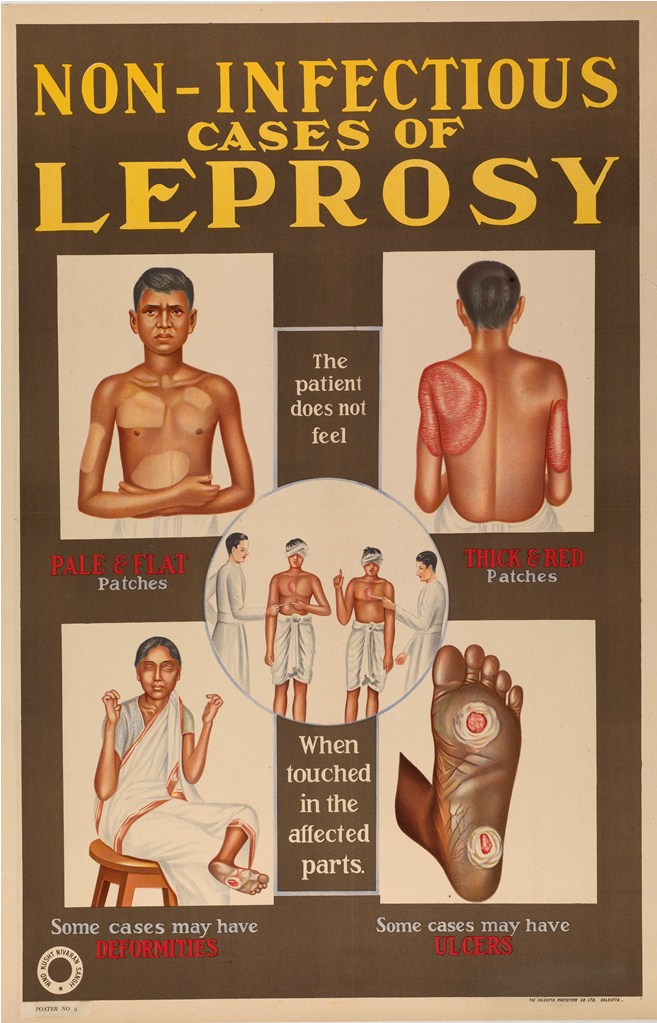
When not treated, leprosy can be severely disfiguring (see photos on this page). This problem, as well as the long history of the disease, are important factors in creating a social stigma around infected people. The stigmatizing of leprosy patients is unfortunate, as it may play a role in reluctance to seek treatment --- and given that treatment quickly renders leprosy uninfectious, the stigma that leads people not to seek treatment has the unfortunate result of helping to spread infeciton.
Although <5% of infected people become ill due to natural resistance to it subclinical leprosy may occur in up to 35% of infected people living in endemic areas (5). The term subclinical means that people may be infected but not have easily observed symptoms of disease. Subclinical infection may present challenges to controlling or eradicating leprosy (6-8).
Dr. GH Armauer Hansen discovered that M. leprae causes leprosy in 1873 (9). Until his discovery, leprosy was thought to be either hereditary or due to miasma. Miasma was basically believed to be bad air in times before germ theory was understood. People miasma was dangerous or capable of causing disease --- the term malaria translates as bad air. Hansen's discovery was the first connection of bacteria to disease. It was greeted skeptically by others and not accepted for several years. However, skepticism that disease could be caused by a microorganism did not stop him from playing a leading role in passing laws that helped prevent the spread of leprosy in his country. Today, leprosy is also called Hansen's disease, in part as a recognition of his work and in part as a effort to de-stigmatize it.
Clinical information
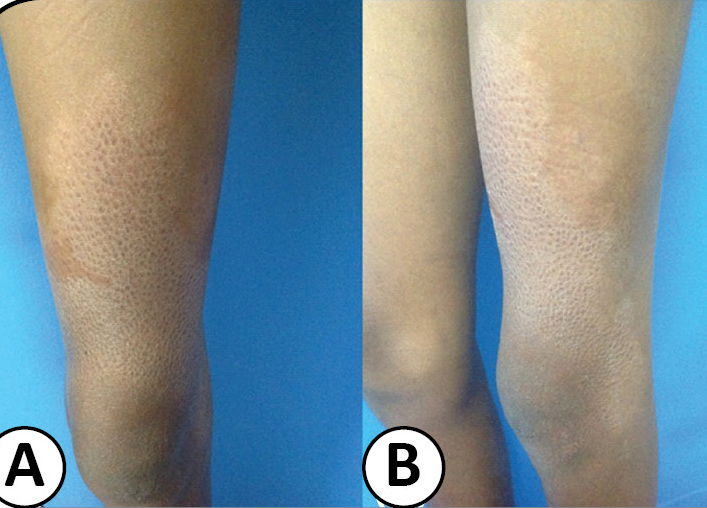
The bacteria that cause leprosy commonly affect a person's skin and peripheral nerves. The most common first problems noticed are one or more skin lesions that may feel numb or that may have reduced sensation. A patient may also feel weak. Skin lesions do not always look the same (see photos and the Diagnosis section below for more information).
The most common signs and symptoms of leprosy are listed below.
- Skin lesions that lose sensation to heat or touch
- Loss of skin pigment in places
- Lost or impaired ability to sweat
- Numbness, pain, tingling in the skin
- Peripheral neuropathy
- Nasal congestion
- Involvement of the eyes
- Loss of sensation in the cornea
- Inability to fully close eyes (lagophthalmos)
- Lesions to the cornea
- Loss of eyelashes
- Loss of eyebrows
- Muscle wasting or atrophy
Common clinical features of DS
Classification of leprosy
There are many different forms of leprosy. The type of leprosy that a person has depends mostly on how his immune system reacts to M. leprae bacteria. All types of leprosy share some features, but there are differences that make them look quite distinct. The variety of types of leprosy has led to systems of classification. These systems simplify diagnosis and provide information to clinicians and field workers in endemic areas. In summary, there are currently two systems for classifying leprosy. An older, more specific system was developed in 1966. This system is called the Ridley-Joplin classification (10). The other system was developed by the World Health Organization (WHO) in 1982 (11).
Ridley-Jopling classification scale
The developers of this scale noted that leprosy occured along a spectrum, with two distinctive forms at either end and intermediate forms in between them. They divided the types of leprsoy into five groups that ranged from tuberculoid to lepromatous. Three intermediate types were defined initially, and a two other types (I and PNL below) were added later:
- Tuberculoid (TT)
- Borderline tuberculoid (BT)
- Borderline (BB)
- Borderline lepromatous (BL)
- Lepromatous (LL)
- Indeterminate (I)
- Pure neuritic (PNL)
The type of leprosy that a patient develops depends on how his immune system reacts to infection with M. leprae. For example, in the LL form, white blood cells called macrophages are not able to kill the bacteria. People with this type of immune response develop a more severe form of leprosy. In the tuberculoid/TT form, there is a good cellular immune response against M. leprae. The immune response is good, but not complete, and a milder form leprosy therefore develops. For detailed descriptions of the different forms of leprosy, see references 5 and 12.
The LL form of leprosy is the more severe form. People with LL leprosy generally have many skin lesions and/or nodules. Because of the infected person's poor immune response, the bacteria multiply and spread through the blood. As a result, skin lesions may appear anywhere on the body, though the bacteria prefer cooler areas, such as the extremities. Lesions may be red or depigmented, and/or may have brown spots in them. If the disease is not treated and progresses, nodules may form. LL patients often experience nasal congestion and nosebleeds. If the disease is not treated, problems may progress and become more serious. They include eye involvement that may lead to blindness, weakness, saddle deformity of the nose (see photo), and disfigurement of the hands or feet (see photo).
At the other end of the spectrum, people with the TT form have single skin lesions or only a few. In people with dark skin loss of skin pigment is most obvious in lesions (see photo at top of page). In people with lighter skin, the lesions may be reddish or coppery colored. They often lack hair, and may be dry or scaly. They may also have neural symptoms. These include loss of sensation, weakness such as foot drop or weakness in the fingers, and/or paralysis.
The pure neuritic (PNL) form of leprosy is characterized by nerve involvement without skin lesions. This form of leprosy can be very difficult to diagnose, as the lack of skin lesions means that clinicians may not think of leprosy.
Multibacillary (MB) and paucibacillary leprosy (PB)
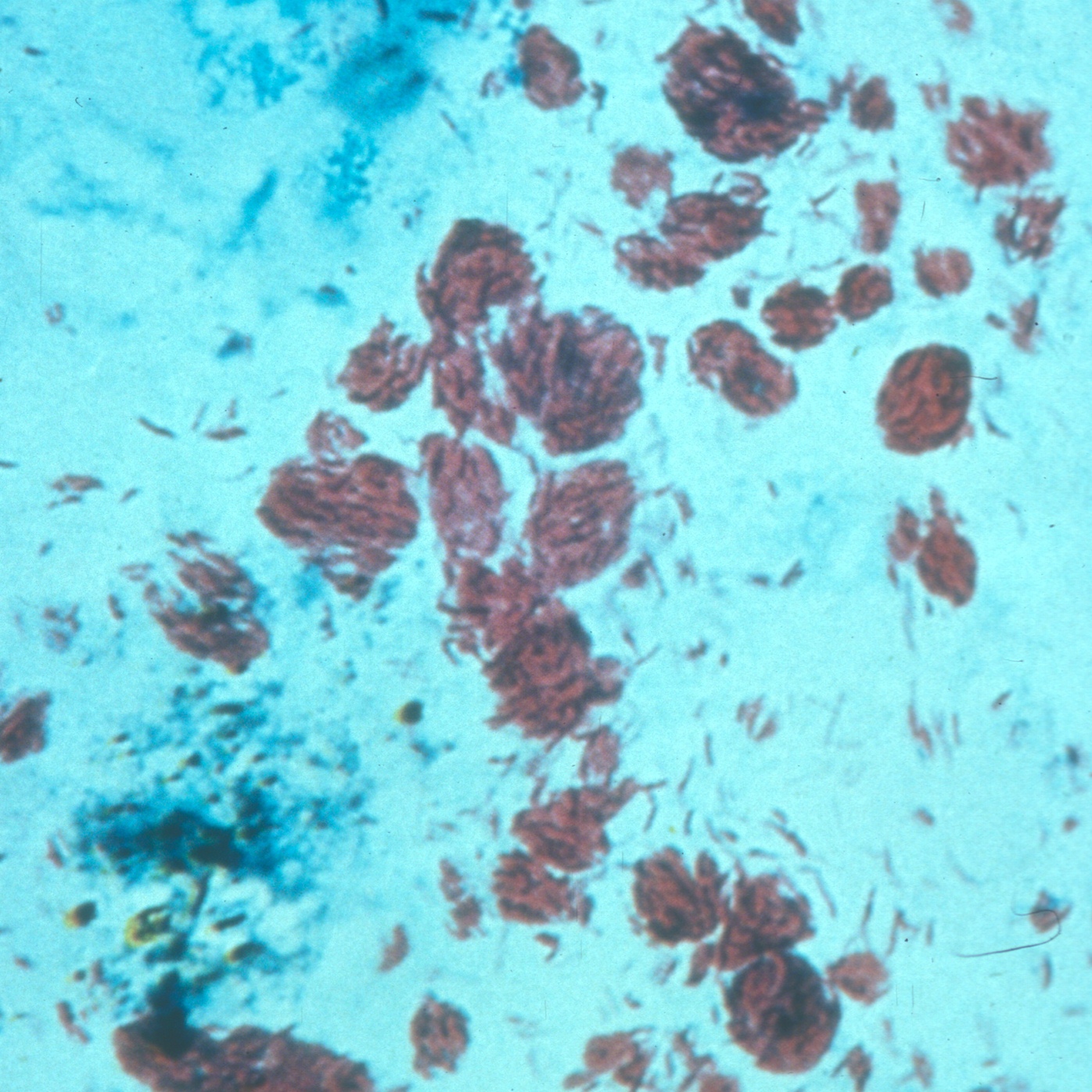
The many forms of leprosy make a specific diagnosis difficult for field workers and rural clinicians who lack even basic testing equipment. As a result, the WHO developed a simplified classification scheme for leprosy in 1982 (11). The scheme was originally based on bacterial load in a patient. Its aim was to simplify diagosis so that trained field workers could make a diagnosis and begin treatment. Initially, workers obtained skin scrapings from patients, smeared them onto slides, and stained them with a substance called Ziehl-Neelsen stain. The stain colors M. leprae bacteria purple, making them easy to see under a basic microscope (see photo on this page).
If bacteria were seen on the stain, the patient was diagnosed with multibacillary (MB) leprosy. If no bacteria were seen and if the patient had fewer than 5 skin lesions, he was diagnosed with paucibacillary (PB) leprosy. The MB forms correlate roughly with the more severe forms on the Ridley-Jopling scale, and the PB forms with the less severe forms. Patients with the MB form are treated with multiple drugs for 12-24 months, and patients with the PB form are treated with two drugs for 6 months.
The WHO now recommends a new system for distinguishing between the MB and PB forms of leprosy. The new system is based simply on the number of skin lesions. Six or more lesions are called MB, 5 or fewer are called PB. This new system is controversial, and a number of studies have found that clinical severity and optimal treatment regimen do not always correlate with the number of skin lesions (13-16).
Type 1 and 2 reactions
Up to half or more of infected people have reactions to leprosy (5). This term means that a person's immune system reacts to dead bacteria. Symptoms of a reaction include pain and swelling of the skin and nerves, although other parts of the body such as the eyes may also be affected. Patients may also be feverish and become swollen. There are two kinds of reactions. They are are called type 1/reversal reactions, and type 2 reactions/erythema nodosum leprosum (12, 17).
In type 1 reactions, skin lesions become red and swollen, and tissue death/necrosis may also occur. Nerves may also be inflamed/swollen and tender; this condition is called neuritis. Neuritis affects nerve function, and if it is not treated, the damage it causes can be permanent. Other problems may also occur, including swelling of the hands, feet, and/or face, and the formation of new lesions on the skin. Type 1 reactions can occur repeatedly, which can cause increasing damage to nerves. They occur most frequently after starting multidrug therapy, but can occur before, during, or after treatment. It is critically important to continue drug therapy when a reaction occurs. The drugs do not cause the reaction. It results from the body's immune system reacting to dead bacteria. Stopping drug therapy can make problems worse. Furthermore, according to the WHO, multidrug treatment reduces both the number and severity of reactions (18).
If a type 1 reaction is mild, it can be treated with painkillers. If nerves are affected, prompt treatment is required to avoid permanent damage. The WHO recommends use of painkillers and corticosteroids, and notes oral prednisolone, 40-60 mg daily (up to a maximum of 1 mg/kg; 18). This treatment usually controls the problem within a few days, and treatment is then tapered off. Treatment should continue for 12 weeks up to 6 months (5, 18).
Newly diagnosed leprosy patients should be given a thorough neurological exam whenever possible. Having a baseline description of the patient's condition will help determine if a reaction is occuring later.
In type 2 reactions, patients may have flu-like symptoms (fever, joint pain, weakness) and warm reddish nodules on the skin (see photo). The nodules are painful and may appear over the entire body. Type 2 reactions are often called ENL reactions. This term is short for erythema nodosum leprosum, which means "red nodules from leprosy" in Latin. ENL reactions can be severe and may affect the eyes, cause arthritis, liver damage, kidney damage, and other problems (5, 12). Tissue death may also occur.
As is the case for type 1 reactions, painkillers and corticosteroids (prednisolone) are used to treat ENL reactions. However, some patients do not respond to prednisolone, and other drugs are needed. Two recommended by the WHO include clofazimine and thalidomide (WHODrugs). Thalidomide is very effective, but it can cause severe damage to a developing fetus. If used in a woman of childbearing age, great care must be taken to avoid pregnancy during treatment, including use of contraceptives and monthly pregnancy testing.
Diagnosis and testing
The diagnosis of leprosy is based on three main factors:
- Skin lesions with loss of sensation (to touch, heat, etc.)
- Thickened nerves
- Skin samples that are positive for acid-fast bacilli
According to the WHO, leprosy can be diagnosed if a person has either skin lesions that are consistent with leprosy OR a positive skin smear. Leprous skin lesions have different forms (see photos on this page). The three most common ones are 1) flat with loss of skin pigment (see photo of woman at top right), 2) raised or flat and copper-colored (border may be indistinct; see photo below), or 3) nodules (see assorted photos to the right and below). The patient typically loses sensation in the nodules, and sweating and hair growth in them may also be reduced or absent. Thickened nerves (see photo of man at right) are common in leprosy, but are not essential for diagnosis. See the photos at right for pictures of skin smears that have been stained to show bacilli. It is important to remember that patients with the neuritic form of leprosy do not have skin lesions.
Males are affected more often than females. The reasons for this difference are not known. In our literature survey, we found sex information on roughly 6,000 patients. Two-thirds of them were male.
Differential Diagnosis
A number of common and uncommon conditions can resemble leprosy. They are listed below.
Arthritis. Nerve pain is a common problem in leprosy, but it is easily misdiagnosed as joint pain due to arthritis. This type of misdiagnosis is more common in areas where leprosy is not common, and is exacerbated by the fact that leprosy causes arthritis in a minority of patients. Clinicians working in endemic areas should check for leprosy in people with joint pain, and should remember that the appearance of skin lesions varies, and that swollen nerves are common. Those outside endemic areas should consider leprosy in a patient with joint pain who has relocated from an endemic area. Given that symptoms may take 20 years to appear, leprosy should be considered even if the move was many years earlier.
Skin conditions. Skin conditions that resemble leprosy include (but are not limited to) tinea versicolor, pityriasis rosea, and erysipelas. Tinea versicolor is a fungus infection that is common in the tropics. The fungus causes lesions with loss of pigmentation. This condition is not painful (though patches may be itchy), and it does not involve the nerves. These characteristics may help distinguish it from leprosy. In pityriasis rosea, red lesions form on the skin; days to weeks later, new smaller "daughter lesions" may appear. They may surround the original lesion or appear in new places. The cause of this condition is not clear, but it seems to heal on its own. Again, the nerves are not involved. Erysipelas is an infection of the skin caused by group A Streptococcus bacteria. Skin plaques are angry red or purple, swollen, and warm. They may blister and be painful, and a patient may develop a fever. It usually affects the lower extremities, but can affect the face, where it forms a butterfly pattern. Erysipelas may be a complication of diabetes, alcoholism, and obesity, and it can occur in pregnant women as well. Onset is usually abrupt. It responds to penicilln antibiotics.
This document from the National Leprosy Eradication Programme (NLEP; India) has an excellent overview of the differential diagnosis for leprosy. NLEP has also produced a document with an overview of the different forms of leprosy in an easy-to-read table.
References
- 1. Robbins G et al. (2009) Ancient skeletal evidence for leprosy in India (2000 B.C.). PLoS One 4(5):e5669. doi: 10.1371/journal.pone.0005669. Full text on PubMed.
- 2. Monot M et al. (2005). On the origin of leprosy. Science 308(5724):1040-1042. Abstract on PubMed
- 3. Mariotti et al. (2005) Probable early presence of leprosy in Europe in a Celtic skeleton of the 4th-3rd century BC. Int J Osteoarch 308(5724):1040-1042. Abstract from publisher.
- 4. Health Resources and Services Administration. Patient information about leprosy. Main page.
- 5. Worobec SM (2009). Treatment of leprosy/Hansen's disease in the early 21st century. Dermatol Ther 22(6):518-537. Abstract on PubMed.
- 6. Godal T & Negassi K (1973) Subclinical infection in leprosy. Br Med J 3(5880):557-559. Full text on PubMed.
- 7. Baumgart KW et al. (1993) Subclinical infection with Mycobacterium leprae--a problem for leprosy control strategies. Trans R Soc Trop Med Hyg 87(4):412-415. Abstract on PubMed.
- 8. Barreto JG et al. (2003) High rates of undiagnosed leprosy and subclinical infection amongst school children in the Amazon Region. Mem Inst Oswaldo Cruz 40(1):34-36. Full text from Scielo.
- 9. Hansen GA. (1874) Undersøgelser Angående Spedalskhedens Årsager (Investigations concerning the etiology of leprosy). Norsk Mag. Laegervidenskaben4:1-88. Locations in WorldCat.
- 10. Ridley DS & Jopling WH (1966). Classification of leprosy according to immunity. Int J Lepr 34(3):255-273. Full text from publisher.
- 11. World Health Organization (1982). Chemotherapy of leprosy for control programmes. World Health Organ Tech Rep Ser 675:1-33. Full text from the WHO.
- 12. Lastória JC & Abreu MA (2014) Leprosy: review of the epidemiological, clinical, and etiopathogenic aspects - part 1. An Bras Dermatol 89(2):205-218. Full text on PubMed.
- 13. Kumar B & Dogra S (2009) Leprosy: A disease with diagnostic and management challenges! relevance to their grouping into paucibacillary or multibacillary disease. Indian J Dermatol Venereol Leprol 75(2):111-115. Full text from publisher.
- 14. Pardillo FE et al. (2007) Methods for the classification of leprosy for treatment purposes. relevance to their grouping into paucibacillary or multibacillary disease. Clin Infect Dis 44(8):1096-1099. Full text from publisher.
- 15. Rao PN et al. (2006) Evaluation of leprosy patients with 1 to 5 skin lesions with relevance to their grouping into paucibacillary or multibacillary disease. Indian J Dermatol Venereol Leprol 72(3):207-210. Full text from publisher.
- 16. Veena S et al. (2011) Significance of histopathology in leprosy patients with 1-5 skin lesions with relevance to therapy. J Lab Physicians 3(1):21-24. Full text on PubMed.
- 17. Walker SL & Lockwood DN (2007) Leprosy. Clin Dermatol 25(2):165-172. Abstract on PubMed
- 18. World Health Organization (1998). WHO Model Prescribing Information: Drugs Used in Leprosy. Geneva; identifier WHO/DMP/DSI/98.1 Full text from the WHO.
- 19. Northern Territory Government; Dep't of Health and Welfare (2010). Guidelines for the control of Leprosy in the Northern Territory 2010. Full text.
- 20. Sette CS et al. (2015) Surgical treatment of type I neuritis in a teenage boy with borderline tuberculoid leprosy. relevance to their grouping into paucibacillary or multibacillary disease. Rev Soc Bras Med Trop 48(2):228-230. Full text from publisher.
- 21. Public health poster; India, 1950s. the Wikimedia Commons..
- 22. Hogeweg M (2010) Leprosy and the eye teaching set. London: International Centre for Eye Health www.iceh.org.uk Photo on Flickr.
- 23. Photo by Bruno Jehle and found on the Wikimedia Commons..
- 24. Hogeweg M (2010) Leprosy and the eye teaching set. London: International Centre for Eye Health www.iceh.org.uk Photo on Flickr.
- 25. Hogeweg M (2010) Leprosy and the eye teaching set. London: International Centre for Eye Health www.iceh.org.uk Photo on Flickr.
- 26. Taheri JB et al. (2012) Oro-facial manifestations of 100 leprosy patients. relevance to their grouping into paucibacillary or multibacillary disease. Med Oral Patol Oral Cir Bucal 17(5):e728-732 Full text on PubMed.