Netherton syndrome
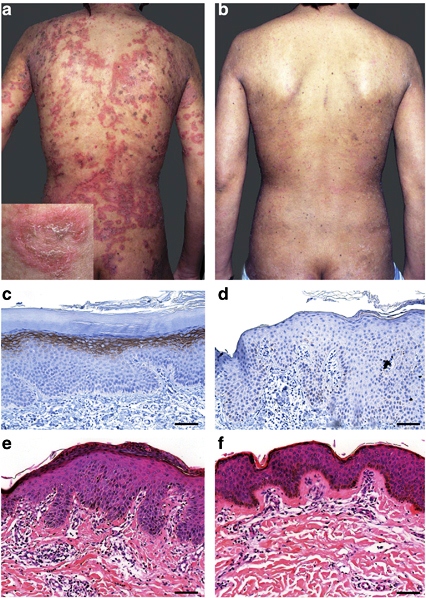
Netherton syndrome (NS) is a congenital disorder that affects the skin, hair, and immune system. An important feature of NS is that most patients are born with congenital ichthyosiform erythroderma, or scaly red skin (see photograph of toddler below on left). Ichthyosis means dry, thickened, scaly skin; and severity varies from mild to severe and disfiguring. Ichthyoses are members of a family of disorders that share ichthyosis. The FIRST Skin Foundation (see link at right) lists 18 different ichthyoses.
It has been estimated that roughly 1 infant in 200,000 is born with Netherton syndrome (1). However, this figure may be an underestimate due to underdiagnosis of NS.
Clinical information
NS typically presents at birth or with a few weeks of birth. As noted above, neonates typically present with scaly/flaky skin that is red and may be angry-looking. Some common medical problems that occur in NS are as follows:
- Feeding difficulties
- Erythroderma at birth (red skin that may be scaly and/or flaky)
- Itchy skin
- Elevated IgE (close to universally present; retesting in negative cases may be advisable)
- Food allergies
- Hay fever or other allergies
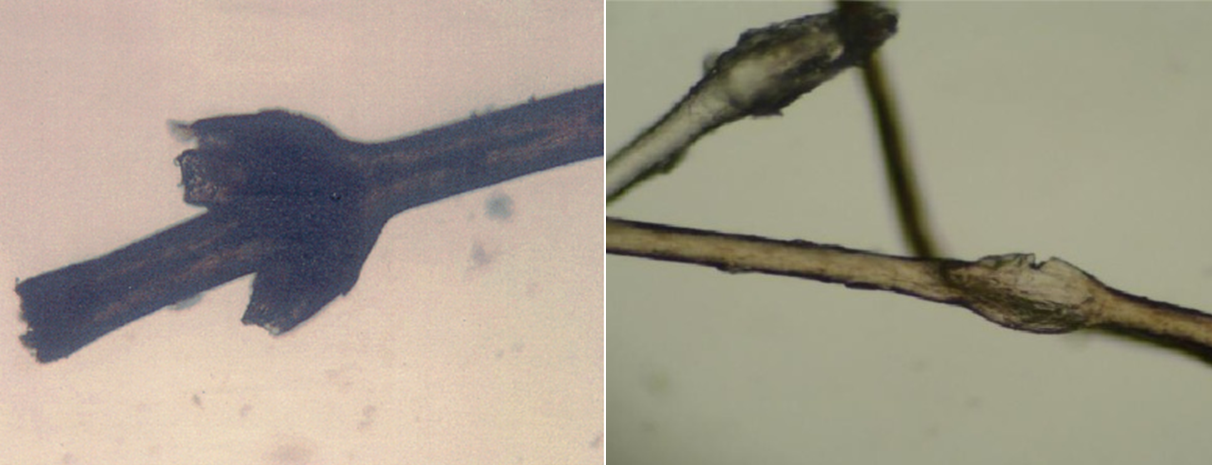
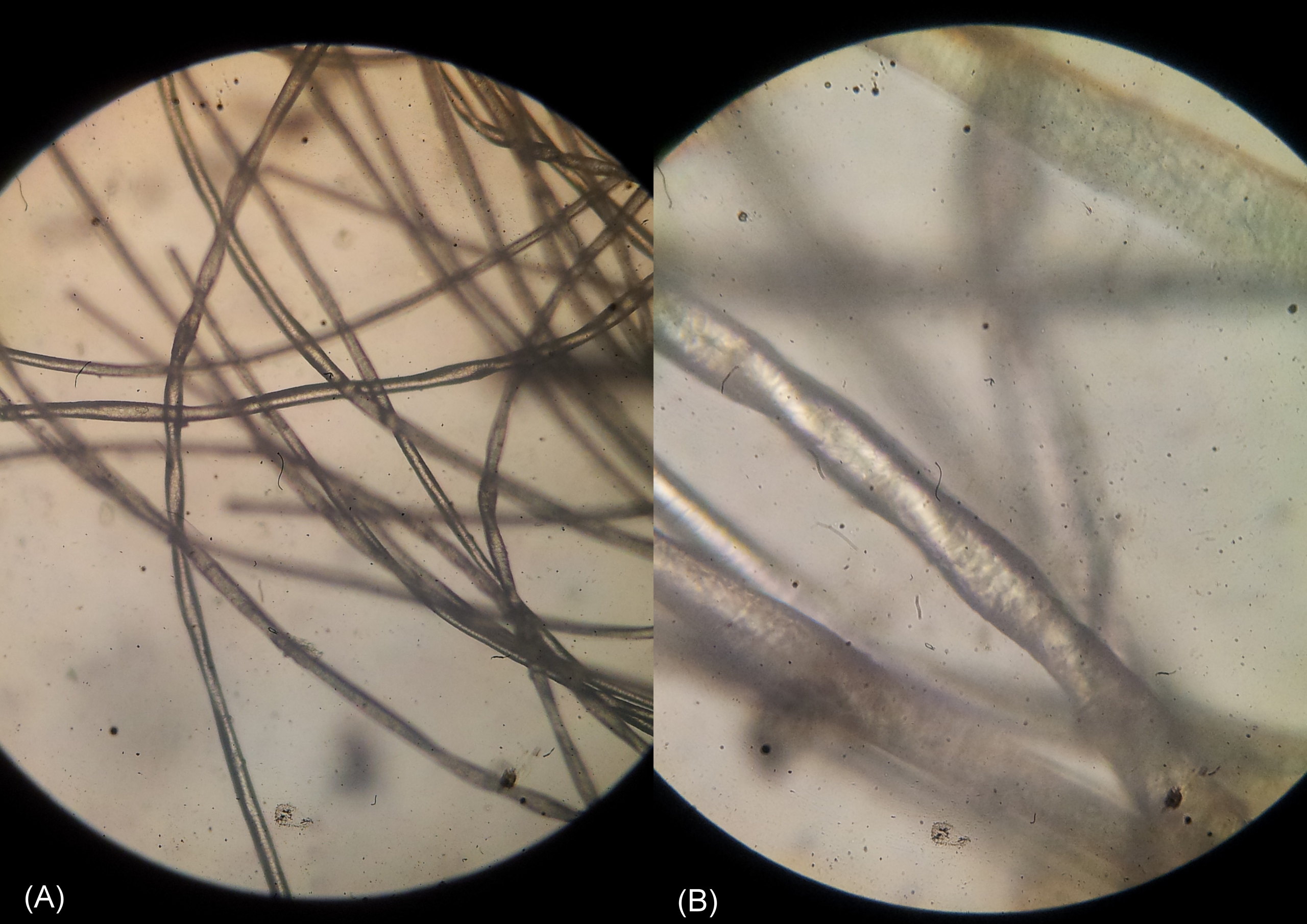
- Hair shaft abnormalities: trichorrhexis invaginata or bamboo hair; see photos below
- Hair shaft abnormalities: pili torti or twisted hair; see photos below
- Brittle hair that does not grow long (may improve with time)
- Dry hair
- Sparse hair
- Ichthyosis linearis circumflexa (ILC; see photo below at right)
- Hyperkeratosis (thickening) of the skin's outer layer
- Eczema-like rash
- Enteropathy (may be life-threatening)
- Hypernatremic dehydration (may be life-threatening)
Common problems in Netherton syndrome
Hair abnormalities are best viewed under a microscope. However, they may not always be present, particularly in children under age 2. It is therefore important to recheck hair if nothing is found. In addition, the eyebrows may be more likely to show trichorrhexis invaginata and/or pili torti. Checking hair and eyebrow samples may be advisable.
Trichorrhexis invaginata and ichthyosis linearis circumflexa are pathognomonic for Netherton syndrome. However, these problems may not become evident until after a patient's first or second birthday. This fact complicates diagnosis in infancy (2). Given that the disease can be lethal, particularly in first year, clinicians may wish to consider NS in any infant presenting with congenital erythroderma, scaling skin, and elevated levels of IgE. Food allergies are also common in NS patients.
Netherton syndrome is an autosomal recessive disorder caused by mutations in the gene SPINK5. Autosomal recessive means that the syndrome occurs when both parents carry a mutated copy of a gene, and each passes the mutated gene to a child. The link at the right under Testing provides a list of laboratories that perform genetic testing for mutations in SPINK5.
A number of other diseases resemble NS. One is trichothiodystrophy (TTD). TTD patients have brittle hair, red skin/sunburns due to photosensitivity, and ichthyosis. In addition, children with TTD tend to be very short and intellectually disabled. These problems also occur in NS, though sometimes to a lesser degree (a majority of NS patients are not intellectually disabled, for example). This fact can make it difficult to distinguish the two conditions. One abnormality that can help in that regard is that a majority of TTD patients are born with a collodion membrane, which is a shiny membrane covering the newborn. The membrane may resemble plastic wrap. NS patients do not appear to have this problem.
Although a number of sources on the internet note that NS infants may be born with these membranes, we have not found a publication citing the problem, althouh we did find a publication refuting the connection (3). We examined 18 publications describing 101 NS patients and did not find any suggestion that a collodion membrane was present at birth. However, three papers describing 27 patients (not including the paper that refuted the connection) specifically noted that a collodion membrane was not present. Thus, the presence of a collodion membrane weighs against NS.
TTD and NS may be also distinguished by differences in their hair. Although both TTD and NS patients have dry, brittle hair, TTD patients have a tiger-tail pattern in their hair under polarized light (may not be present at birth). NS patients do not have this abnormality. Note that trichorrhexis nodosa (paintbrush hair) is very common in TTD; it also occurs in NS, although in a minority of patients.
Pathological photosensitivity is also not a feature of NS; clinicians wishing to rule out TTD in fair-skinned patients who burn easily may wish to arrange for UV sensitivity testing of fibroblasts or have a sequencing test performed. Sequencing is generally the easier of the two options by far.
Netherton syndrome is also very similar to congenital ichthyosiform erythroderma (CIE). CIE patients are born with the same skin condition that affects NS patients. NS and CIE are caused by mutations in different genes, and as many as 90% of CIE patients are born with collodion membranes, a problem that does not appear to affect NS patients (4).
The skin manifestations in a number of other conditions resemble those in NS. These other conditions include psoriasis, seborrheic dermatitis, exfoliative dermatitis, and atopic dermatitis. However, most other medical problems associated with NS do not generally occur in these conditions. They include intellectual disability, short stature, hair abnormalities, and failure to thrive.
NS is usually treated with a variety of skin emollients and moisturizers. According to the NORD article linked to on the right, treatment should be tailored individually to each patient, as some agents (such as cortocosteroids) may contain ingredients that can enter the bloodstream and endanger the patient (especially if he is a child). Antihistamines can help with itching. Antibiotics (both topical and systemic) may necessary to control infections, as the skin abnormalities in NS make patients vulnerable to infection.
At this time, there are no FDA-approved treatments for Netherton syndrome. However, researchers have published small studies of off-label treatments that appear to improve skin problems in a limited number of patients. For example, infliximab (trade name: Remicade) is approved by the FDA for the treatment of a number of conditions including Crohn's disease, ulcerative colitis, two forms of arthritis, and others. Infliximab is a monoclonal antibody used as an infusion on a dosing schedule that generally resembles a treatment at 0, 2, 6 weeks, and then every 8 weeks. Side-effects can be significant (5). The NS study was performed in one patient only (6).
Another experiment treatment for NS involved treating five patients with intravenous immunoglobulin (7). The authors reported the following clinical benefits:
- Decreased inflammation
- Decreased itching
- Thicker hair
- Fewer broken hair shafts
- Healthier scalps
Intravenous immunoglobulins have been used since 1952, and are approved for the treatment of a variety of medical conditions (8). However, NS is not among them, and the study above has not been repeated to the best of our knowledge.
A variety of other compounds have been used experimentally for NS. Interested readers may wish to look at search results for treatment of netherton syndrome in Google scholar.
References
- 1. Prevalence estimate stated in Netherton syndrome: Genetics Home Reference
- 2. Fartasch M et al. (1999) Altered lamellar body secretion and stratum corneum membrane structure in Netherton syndrome. Arch Dermatol 135(7):823-833. Full text from publisher.
- 3. Larrégue M & Guillet G (2007) Collodion baby with neonatal signs of trichothiodystrophy misdiagnosed as Netherton syndrome: reassessment of a previous diagnostic error. Ann Dermatol Venereol 134(3 Pt 1):245-248. Abstract on PubMed.
- 4. Richard GB & Bale SJ (2001) Autosomal Recessive Congenital Ichthyosis. Updated August 28, 2014. GeneReviews [Internet] Pagon RA et al., editors. Seattle (WA): University of Washington, Seattle; 1993-2021. Full text.
- 5. Side effects noted in Full prescribing information.
- 6. Fontao L et al. (2011) Infliximab Infusions for Netherton Syndrome: Sustained clinical improvement correlates with a reduction of thymic stromal lymphopoietin levels in the skin. APSP J Inv Dermatol 131:1947-1950. Full text from publisher.
- 7. Renner ED (2009) Comèl-Netherton syndrome - defined as primary immunodeficiency. J Allergy Clin Immunol 124(3):536-543. Full text on PubMed.
- 8. Gelfand EW (2012) Intravenous immune globulin in autoimmune and inflammatory diseases. NEJM 367(21):2015-2025. Abstract on PubMed.
- 9. Dey VK (2011) Netherton syndrome: A rare genodermatosis. Indian Derm Online J 2(1):38-39. Full text on PubMed.
- 10. Ng E (2014) Netherton syndrome with ichthyosis linearis circumflexa and trichorrhexis invaginatum. Derm Online J 20(12):pii: 13030/qt7m95t6v6. Abstract on PubMed. Full text from publisher.
- 11. Srinivas SM et al. (2013) Netherton Syndrome with Pili Torti. Int J Trichology 5(4):225-226. Full text on PubMed.
- 12. Duquia RP et al. (2006) Netherton's syndrome with a 20-year follow-up. An Bras Dermatol 81(6):559-562. Full text.
- 13. Boskabadi H et al. (2013) Netherton syndrome, a case report and review of literature. Iran J Pediatr 23(5):611-612. Full text on PubMed.
- 14. Ghosh S et al. (2012) Menkes kinky hair syndrome: A case report. Derm Online J 18(11):4. Full text from publisher.