Cri Du Chat Syndrome (CdCS)
Clinical information
Cri du Chat Syndrome, also known as cat's cry syndrome, 5p minus syndrome or LeJeune's syndrome, is a rare chromosomal disease (1-3). It is thought to occur in one in 15,000 to 50,000 births (4, 5) and is somewhat more common in females than in males, with roughly 60% of patients being female (reviewed in 1). CdCS occurs in people of all ethnicities.
The most frequent clinical sign of CdCS is an unusual high-pitched and/or weak cry that sounds like a cat meowing. This cry gives the syndrome its name (click on the Multimedia link on this page for an example). This unusual cry is happens in a large majority of patients and is typically recognizable at birth.
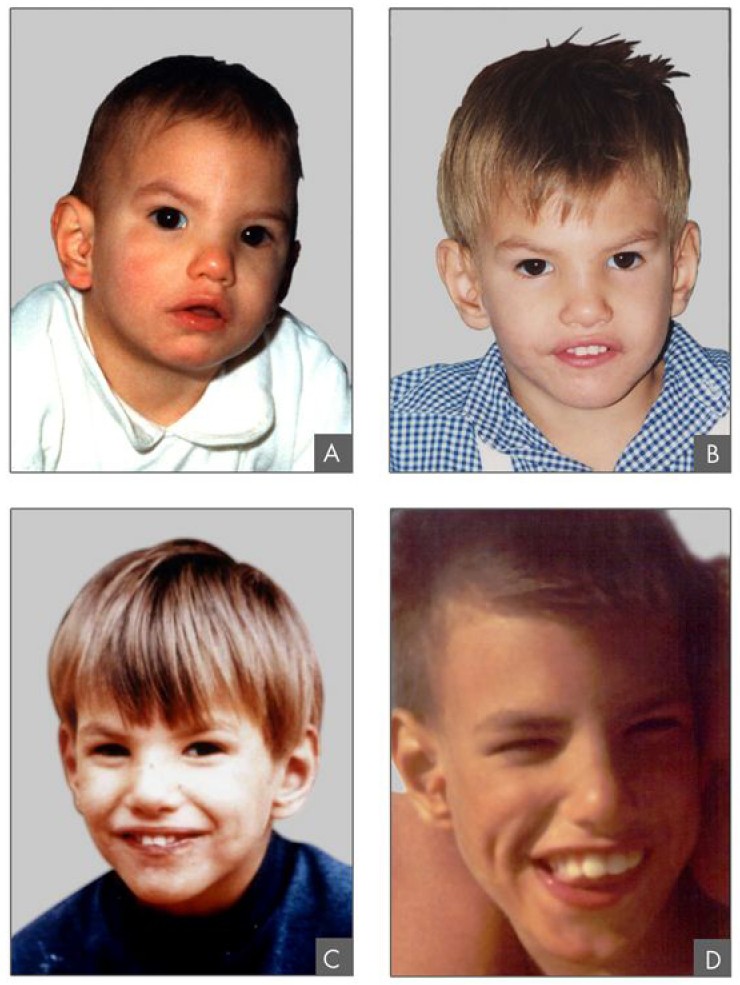
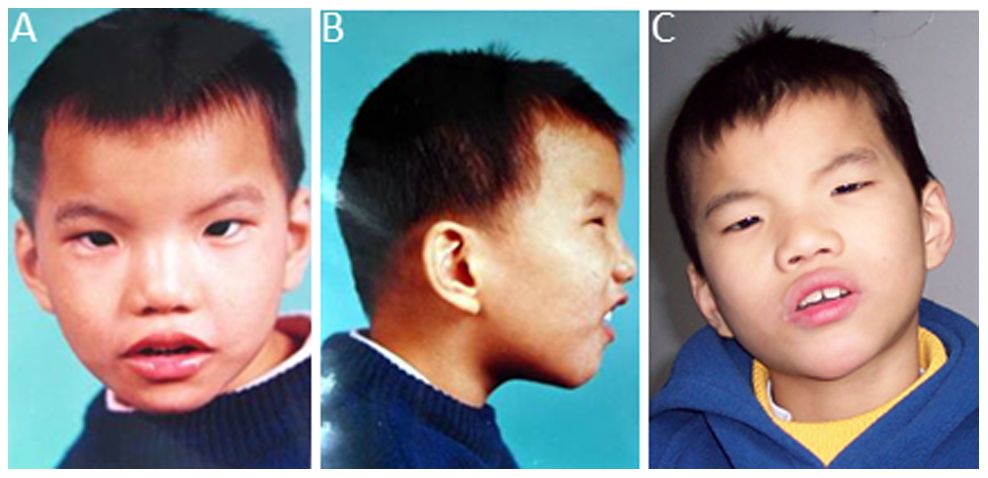
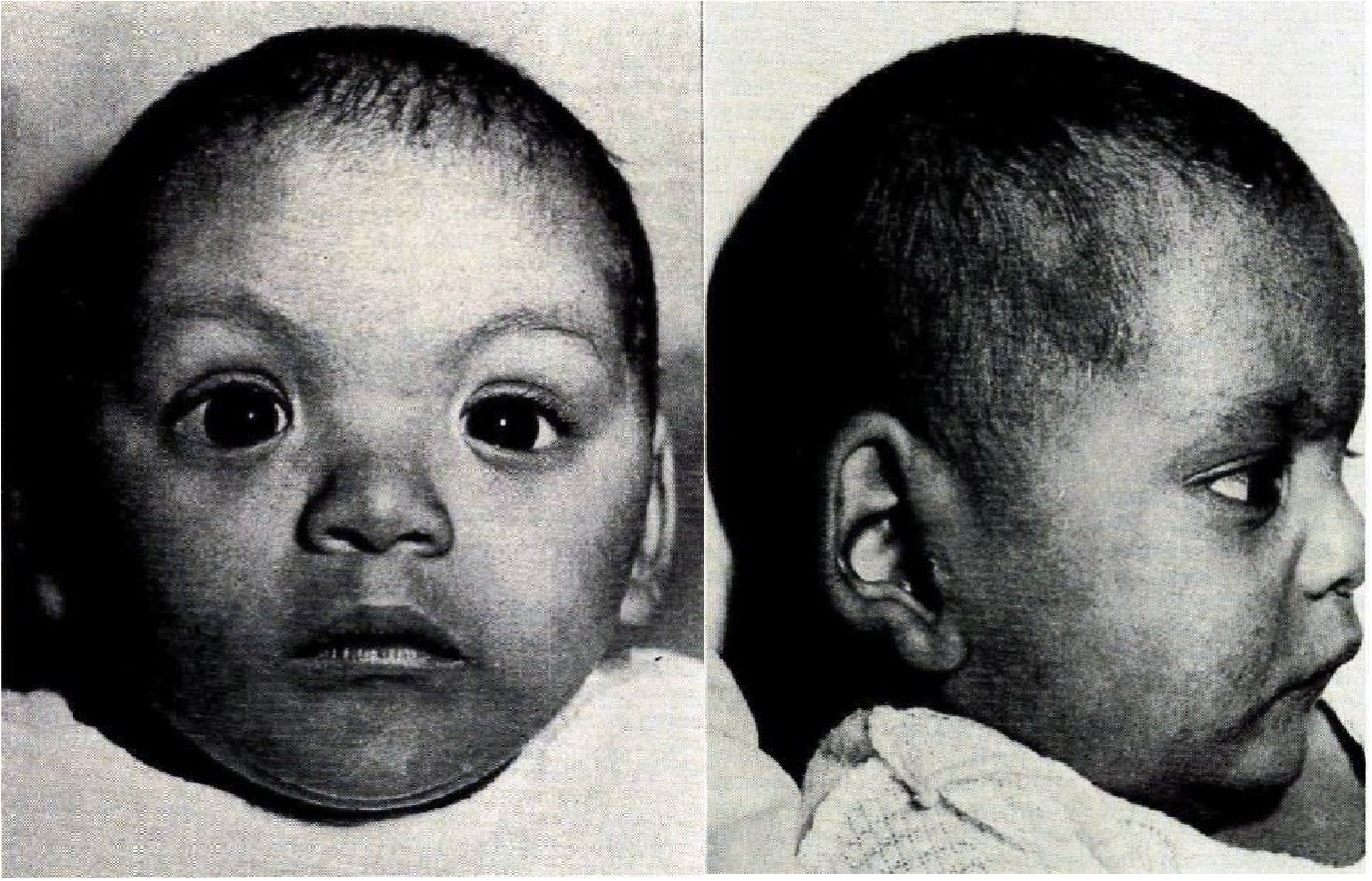
Many of the most common clinical signs of CdCS are neurodevelopmental (see list below and reference 1). Infants are usually small at birth (especially as regards weight). Many patients with CdCS have a distinctive facial appearance. For example, they may have skinfolds in the inner corers of their eyes (epicanthal folds, which are typical in healthy people of east Asian origin), low-set and misformed ears, and asymmetry of the face. In addition, infants with CdCS may have round faces in infancy that become more elongated with time. A small head/microcephaly, a small and backward slanting lower jaw, and hypotonia/floppy muscles are also common. In addition, speech development tends to be delayed, as are gross motor skills.
People with CdCS usually lose the cat-like cry during the first two years of life, though they may retain other vocal features such as hoarseness or a weak, high-pitched voice. As patients age, they typically lose the rounded face and develop a narrow, elongated face and more marked microcephaly, as seen in the photo at the right (2). May people develop dental anomalies.
It is important to note that the degree and type of symptoms are variable between different individuals. Some patients with a confirmed diagnosis have few of the features associated with the disease and may appear nearly normal. This fact explains the wide range in estimates of the CdCS's rate of occurrence.
People with milder forms of CdCS may not be diagnosed during infancy if the unusual cry is not present or not recognized. Behavioral signs, motor delays, and nonspecific intellectual disability or speech impairments are usually present to some degree in these patients. Therapeutic interventions in early childhood may help the level of skill development. Children with CdCS may benefit greatly from interventions intended to improve psychomotor/social skills and communication, so timely diagnosis is important (1, 3). Clinical features that occur in Cri du Chat Syndrome include the following:
- A cry that resembles that of a kitten meowing: typically high-pitched and mewling
- Self-harming behaviors (hairpulling, biting, or head-banging)
- Sensitivity to sounds in particular frequency ranges
- Intellectual disability/low IQ (mild to severe)
- Balance problems, falls, and/or clumsiness
- A single crease on the palm of the hand
- Foot deformities (flat feet or clubfeet)
- Delayed development of motor skills
- Feeding or swallowing difficulties
- Hypotonia/floppiness in infancy
- Delayed speech development
- Short fingers (brachydactyly)
- Fused fingers (syndactyly)
- Tantrums and aggression
- Prematurely grey hair
- Failure to thrive
- Low birthweight
Common clinical features of cri du chat syndrome
A number of other problems may also occur in CdCS. They include congenital heart defects, kidney defects, brainstem abnormalities, hip problems, hypermobile joints, sleep disorders, undescended testicles, hyperactivity, respiratory distress, frequent infections, and abnormal curvature of the spine (1-3).
People with cri du chat syndrome also have distinctive facial features (see photos on this page), as listed below:
- A rounded face in infancy that becomes elongated as a patient ages
- Epicanthal folds (skin folds over the inner corners of the eyelids)
- Receding jaw/retrognathia
- Small jaw/micrognathia
- Flattened nasal bridge
- An asymmetric face
- Wide-set eyes
- Deformed ears
- Low-set ears
Common facial features of CdCS
Life expectancy with CdCS is usually normal with the exception that infant mortality has been estimated to be as high as 10%, with one older study (1978) reporting that most infants who died succumbed to respiratory infections or cardiac defects in the first months of life (4). This information has not been updated and it is not clear if general advances in medicine since the 1978 have reduced infant mortality in CdCS.
Syndrome-specific growth charts exist for CdCS. Please visit our Italy page for links to the charts (syndrome-specific growth charts are at the bottom of the page).
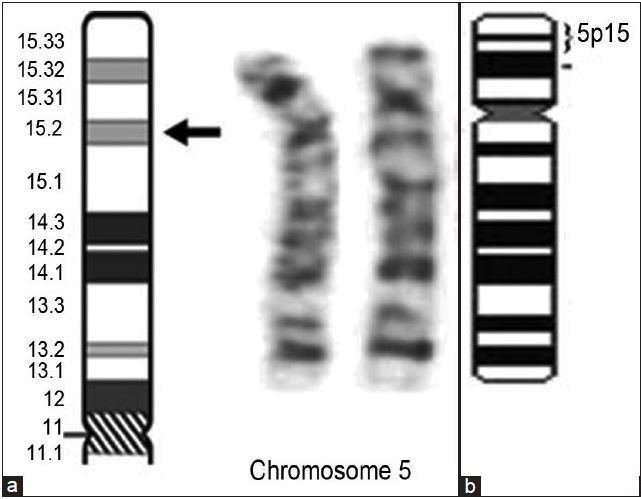
Cause
CdCS is caused by the total or partial deletion of a part chromosome 5 called the short arm (6). Most cases are due to de novo deletions, meaning that they happen spontaneously and there is no family history of the disorder (7). In these cases, the risk of having an affected sibling is low. However, roughly 10-15% of cases are due to what is called a balanced translocation, a situation that may increase the risk of having another child with CdCS (discussed in 8). Chromosomal analysis and counseling with a genetics professional can help determine if this risk exists. Females with CdCS have a high chance of having an affected child, and again, counseling with a genetics professional is important.
Diagnosis and Testing
A history of the distinctive cry of CdCS tends to be the most important sign aiding diagnosis. In cases where the cry has not been observe, diagnosis may be delayed because a patient's other features are not distinctive enough to make a diagnosis. A review of CdCS has noted that clinical diagnosis depends "more on the ability to recognize the combination of a collection of more or less specifc [features] (microcephaly, facial dismorphism, typical cry, low weight in birth, etc…) rather than on the futile seeking of the pathognomonic signs of the syndrome rather than on the futile seeking of the pathognomonic signs of the syndrome" (1).
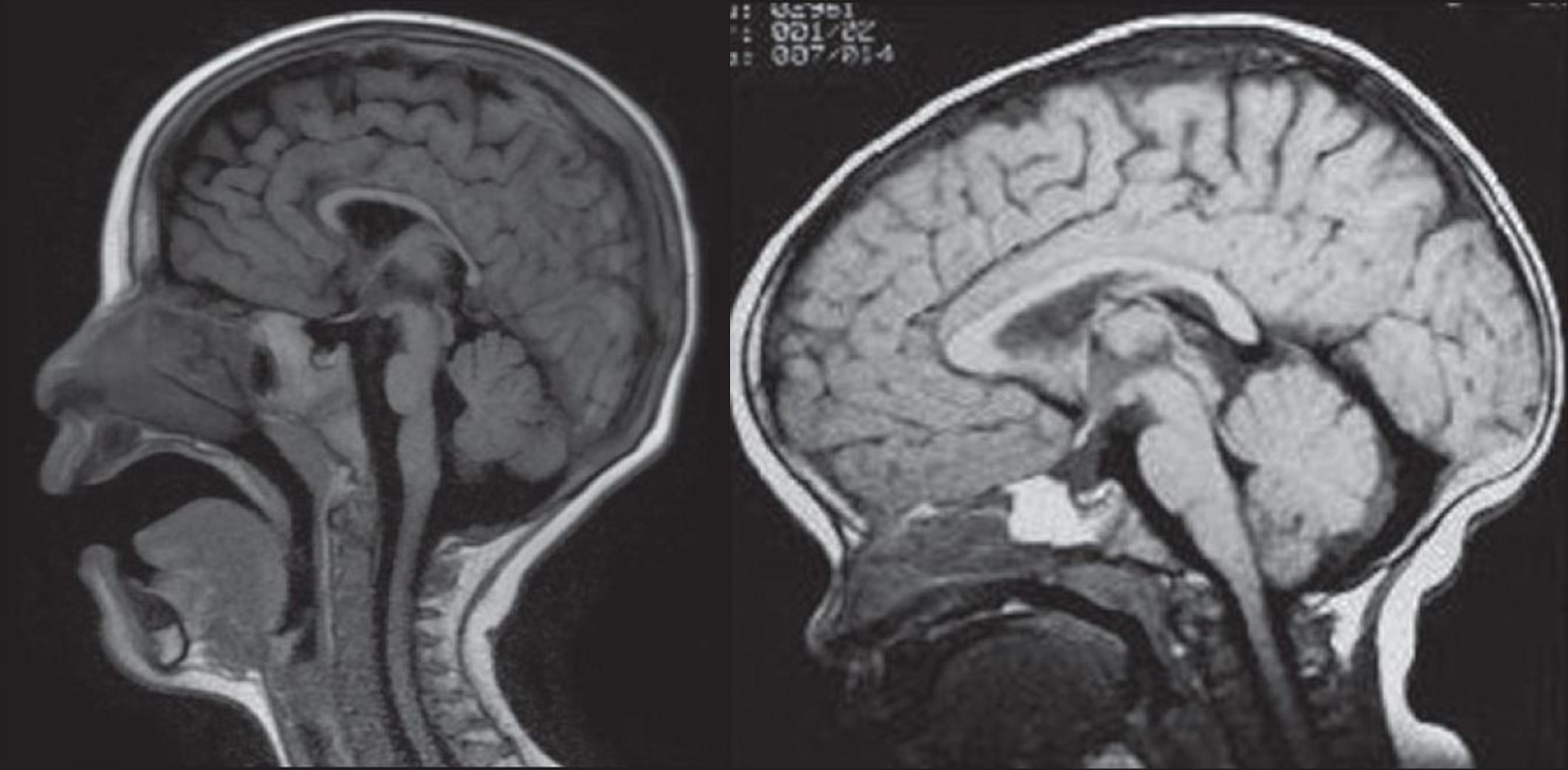
One important tool in diagnosis may be T1-weighted MRI imaging, as shown in the images on this page. The brainstem, pons, and/or cerebellum of patients with CdCS may show significant hypoplasia in MRI images as compared with age-matched healthy children (9).
Many instances of CdCS are the result of deletions that are large enough to be evident on a karyotype, without additional detailed analysis (see sample karyotype of a deletion on chromosome 5 at right; 10). As noted above, in some cases, additional testing may be advised in order to determine if there is a substantial risk of having another affected child.
Differential Diagnosis
While only the unusual cat-like cry is distinctive in CdCS, the combination of features (see list above) can create a diagnostic picture, particularly over time. In the absence of the distinctive cat-like cry during infancy, the features of CdCS may resemble several other conditions, as described below.
Fetal alcohol syndrome (FAS). Infants with CdCS may have facial features and developmental delays that resemble those of FAS. One difference lies in the philtrum (the groove below the nose). In CdCS, the philtrum is short while children it tends to be long in FAS, and smooth as well. Children with fetal alcohol exposure also tend to have a thin upper lip. A history of alcohol use in pregnancy can help distinguish the two conditions.
Cohen syndrome. Children with this syndrome may have hypotonia/floppy muscles, failure to thrive, microcephaly, joint hypermobility, and psychomotor delays beginning in infancy, as children with CdCS do. however, patients with Cohen syndrome generally do not have the pattern of facial feature seen in CdCS, and vision problems that are common in Cohen syndrome are unusual in CdCS.
Wolf-Hirschhorn syndrome (Wolf syndrome). Like CdCS, Wolf-Hirschhorn syndrome is caused by deletion of part of a chromosome (the short arm of chromosome 4p in this case). Many features are shared by the CdCS and this syndrome: low birth weight, short stature, hypotoniafloppiness, and developmental delays. The two syndromes also share a number of facial features, including wide-set eyes, epicanthal folds, a wide nasal bridge, a downturned mouth, and malformed ears. However, the cat-like cry that is so common in CdCS does not appear to be a feature of Wolf-Hirschhorn syndrome. Laboratory testing may be required to distinguish the two conditions.
References
- 1. Rodriguez-Caballero A et al. (2010) Cri du chat syndrome: A critical review. Med Oral Patol Oral Cir Bucal 15(3):e473-478. Full text from publisher.
- 2. Mainardi PC (2006) Cri du Chat syndrome. Orphanet Journal of Rare Diseases 1:33. doi: 10.1186/1750-1172-1-33. Full text on PubMed.
- 3. Sigafoos J et al. (2009) Editorial: Cri-du-Chat. Dev Neurorehabil 12(3):119-121. Abstract on PubMed.
- 4. Niebuhr E (1978) The Cri du Chat syndrome: epidemiology, cytogenetics, and clinical features. Hum Genet 44(3):227-275. Abstract on PubMed.
- 5. Higurashi M et al. (1990) Livebirth prevalence and follow-up of malformation syndromes in 27,472 newborns. Brain Dev 12(6):770-773. Abstract on PubMed.
- 6. Lejeune J et al. (1963) 3 cases of partial deletion of the short arm of a 5 chromosome C R Hebd Seances Acad Sci 257:3098-3012 Abstract on PubMed.
- 7. Mainardi PC et al. (2001) Clinical and molecular characterisation of 80 patients with 5p deletion: genotype-phenotype correlation. J Med Genet 31(3):151-158. Full text on PubMed.
- 8. Gu H et al. (2013) A familial cri-du-chat/5p deletion syndrome resulted from rare maternal complex chromosomal rearrangements (CCRs) and/or possible chromosome 5p chromothripsis. PLOS ONE 8(10):e76985. doi: 10.1371/journal.pone.0076985. Full text on PubMed.
- 9. Uzunhan TA et al.(2014) A clue in the diagnosis of Cri-du-chat syndrome: Pontine hypoplasia. Ann Indian Acad Neurol 17(2):209-10. Full text on PubMed.
- 10. Dangare HM et al. (2012) Cri du chat syndrome: A series of five cases. Ind J Pathol Microbiol 55(4):501-505. Full text from publisher.
- 11. Weinkove C et al. (1967) The cat-cry syndrome. South African Medical Journal. 11:218-220. Abstract on PubMed. Full text from Sabinet.