Rett Syndrome (RTT)
Rett syndrome, which is often called RTT for short, is a neurological condition that almost always affects girls, although it occurs rarely in boys. RTT is a member of a large family of neurodevelopmental disorders, which are conditions that cause problems with intelligence and behavior. These conditions may be genetic, acquired, or environmental.
Clinical Information
Most children with RTT are normal at birth and develop normally for at least six months. At some point, most commonly between the ages of 7 and 18 months, problems appear. Head growth may begin to slow and development stagnates. Next, skills that had been acquired are lost, with speech, walking, and use of the hands being affected. A child may be unable to feed or dress herself. She may lose her ability to pick up toys or play with them. This situation does not necessarily mean that she is not interested in toys or in the world around her, but that she cannot interact with it in the ways she wishes to. At the same time, patients develop what are called stereotypic hand movements. This term refers to purposeless, repetitive movements, such as hand wringing or squeezing, handwashing movements, clapping, and/or mouthing (1).
Although skills are lost in RTT, Rett syndrome is not a degenerative disorder. As noted above, it is called a neurodevelopmental disorder. A more precise term describing it would be developmental arrest. This fact means that there may be therapies that can help RTT patients. For example, physical therapy can help patients maintain or regain skills (see Types of RTT, below, for more information).
There are a number of clinical features associated with Rett syndrome. The most common ones are listed below.
- Developmental regression; this condition plateaus/stabilizes later
- Stereotypic hand movements (see photos and videos)
- Loss of speech skills (including babbling)
- Loss of purposeful hand use
- Lost or impaired walking ability
- Intense eye gaze (see photo below)
- Stereotypic behavior (rocking, etc.)
- Truncal ataxia
- Seizures
- Abnormal EEG
- Screaming spells
- Anxiety or agitation
- Frequent laughter (daytime)
- Frequent laughter (nighttime; may last for hours)
- Breathing abnormalities, including breath holding
- Very small head (microcephaly)
- Slowing of head growth
- Very short stature
Common clinical features of Rett syndrome
Scoliosis and other spinal column deformities are very common in RTT. The median age at onset is 9.8 years, with ~75% of patients affected by age 13 (2). Guidelines for managing these problems have been developed (2); there is also a summary of them. Overall, the spine should be examined when a person is diagnosed with RTT, and at six-month intervals after that (with X-rays). Physical therapy is recommended to keep patients walking as long as possible, keep joints mobile, and maintain muscle strength. Braces and surgery may be required.
People with RTT may live into middle age or even old age. However, sudden death occurs in this population at a rate that is somewhat higher the general population's. Cardiac problems occur in RTT may contribute to early morality (reviewed in reference 3). In particular, patients may have alterations in the electrical conduction in the heart (specifically, ventricular repolarization; 3). The cause of this problem is not known, but it can be detected with an ECG/EKG. In addition, abnormalities in the autonomic nervous system may also create heart problems in RTT. The organization Rettsyndrome.org recommends that children with RTT see a cardiologist by age 5 and that an ECG be performed at that time and every other year if results are normal. If results are abnormal, consultation with a cardiologist who is an expert in the heart's electrical function is recommended.
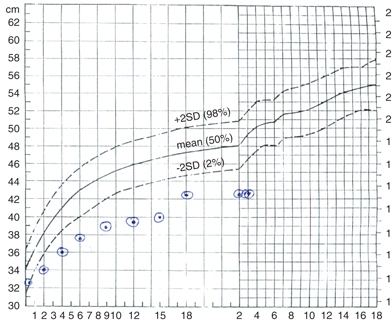
People with RTT tend to be short with small heads. An important feature of RTT is that head growth may be initially normal in an infant, but may slow down (decelerate). Roughly 3/4 of RTT patients have microcephaly. However, girls with a milder form of RTT called the preserved speech variant are generally taller and have larger heads than most others with RTT. Growth charts for Rett syndrome have been made. They are freely accessible via PubMed.
Rett syndrome has been divided into four stages, as described below (source: NIH). These stages apply best to patients with the classic form of RTT (see below).
- Stage 1 (early onset). Development slows; signs may be subtle and easy to overlook at first. Eye contact may falter and there may be less interest in toys. Milestones (sitting, crawling) may be delayed. Head growth may or may not slow in this stage, and repetitive hand movements may or may not appear. This stage can last for a few months to a year.
- Stage 2 (rapid destructive). The child loses purposeful hand motions and language skills. Stereotypic hand movements appear or become more obvious; they disappear when the child is sleeping. Walking is impaired and slow head growth is typically noted. Patients may have autistic-like behaviors, but autism is not a formal feature of RTT. This stage may last for weeks or months and usually starts between ages 1 and 4.
- Stage 3 (plateau). At this stage, seizures and apraxia (difficulty initiating movement) appear. Children may cry less than they had before, and autisic-like behaviors may improve. A patient may be more alert show more interest in her environment. Attention span and communication may also improve. This stage often begins between ages 2 and 10. It may last for years or the rest of the patient's life.
- Stage 4 (late motor deterioration). In this stage, mobility is reduced due to scoliosis and muscle weakness & rigidity. Patients who could walk may lose this skill and they may hold their arms, legs, or upper body in abnormal positions. Skills that do not decline include communication, cognitive ability, and hand skills. Hand stereotypy may decrease and eye gaze may improve.
Types of RTT
There are two general types of RTT: classic and atypical. There is a single classic form and a number of variant forms (preserved speech variant, early seizure variant, and congenital variant). Roughly 75% of RTT cases are classic (4), with the different forms of atypical RTT comprising the rest. In both types of RTT, there is a regression period during which a patient loses skills that had been gained, followed by a period during which the condition plateaus or even improves. Physical, occupational, and other therapies are important for helping patients regain lost skills as much as possible (5). Physical therapy and activity may also help slow physical problems like scoliosis (6).
Diagnostic criteria for RTT are listed in the next section. There is considerable overlap between the two forms of this syndrome. In the classic form, patients lose hand skills, speech, and the ability to walk. Losses may complete or only partial. In cases with younger onset, young children may only have acquired babbling or other very basic speech skills that are then lost. As patients lose purposeful use of their hands, they also develop stereotypies, which are repetitive movements. Hand stereotypies in RTT include handwashing, in which the patient appears to be washing her hands in the air, squeezing, wringing, clapping, tapping, or mouthing of hands (1). They also have gait abnormalities. A very small number of boys with classical RTT have been described in the literature (7).
The forms of atypical RTT differ. For example, the preserved speech variant (also called the Zappella variant) is a milder form of RTT. Girls with this variant have speech abilities that range from single words (at least 10) to the ability to combine words (8). They may also retain manual abilities, such as an ability to draw or write simple sentences, although purposeful hand motion may be lost in this group as well. Other problems generally associated with RTT may or may not occur in this group, or may be milder if they do (8).
In contrast, the congenital variant (also called the Rolando variant) is a more severe form of RTT. This form of RTT has been described in boys (9, 10). Children with the congenital variant are floppy/hypotonic during the first few months of their lives. Unlike most other RTT patients, they may not meet early developmental milestones. They tend to be severely affected. This variant was first described in 1985 (11).
The early-onset seizure variant is characterized by early seizures, with onset usually between age 7 days and 5 months. It was first reported in 1986 and a number of case histories have been published since then (12, 13). Like children with classical RTT, those with this variant have hand stereotypies and impaired psychomotor development. Before seizures develop, they may also have severe hypotonia, and irritability, drowsiness, or feeding difficulties related to poor sucking (14).
Diagnosis and Testing
Diagnostic criteria for RTT have been established and are periodically refined as researchers and clinicians learn more about the syndrome. The most recent criteria were published in 2010 (1). They have been reproduced below. In the past, decleration of head growth (see figure below) was a criterion for diagnosing RTT. This requirement was removed in the latest evaluation of RTT diagnostic criteria (1). However, a diagnosis of RTT should be considered if slowed head growth is observed.
Clinical feature |
|
Required
|
A period of developmental regression followed by recovery or stabilization All main criteria below All exclusion criteria below |
Required
|
A period of developmental regression followed by recovery or stabilization At least 2 of the 4 main criteria below 5 out of 11 supportive criteria |
Main criteria |
Partial or complete loss of acquired purposeful hand skills Partial or complete loss of acquired spoken language Gait abnormalities: loss or dyspraxia/impairment Stereotypic hand movements |
Supportive
|
Breathing disturbances when awake Grinds teeth while awake Impaired sleep patterns Muscle tone abnormalities (hypotonia that may develop into rigidity) Peripheral vasomotor disturbances Scoliosis/kyphosis Growth retardation Small, cold hands and feet |
Exclusion
|
Brain injury secondary to trauma, neurometabolic disease, severe infection* Grossly abnormal development (age <6 months) ** |
*Brain injury that occurs around the time of birth or in infancy; severe infection that causes neurological problems. The evidence that injury caused neurological damage should be clear, such as in a neurological or ophthalmological exam, and via MRI or CT scan (1).
**Here, the term grossly abnormal means that that early milestones such as head control, swallowing, or the development of a social smile are not met. Mild generalized floppiness/hypotonia and other subtle developmental problems have been commonly reported before age 6 months of age in RTT; these milder problems do not exclude a diagnosis of RTT (1).
Diagnosing atypical RTT may be easier in older children. This is because certain features the supportive criteria are age-dependent. Note any history of any of these criteria is sufficient for a yes answer; the feature need not be present at or around the time of examination. Children under age 5 with 2 or fewer supportive criteria should be monitored and reassessed periodically (1).
Diagnostic criteria specific for the preserved speech (8) and early-onset seizure variants (14) have been published.
Causes of RTT
RTT may be caused by mutations in one of three different genes: MECP2 (15), FOXG1 (16), and CDKL5 (17-19).
Roughly 95-97% of cases of classic RTT are caused by mutations in MECP2 (20). No mutation is found in the remaining cases. MECP2 mutations have also been found in the preserved speech variant (21). The early-onset seizure variant is associated with the gene CDKL5 (17-19), and the congenital variant is associated with the gene FOXG1 (16).
MECP2 is located on the X chromosome. This is why RTT occurs almost exclusively in girls: girls have two X chromosomes, but only one of them is active in any given cell. This means that girls have an active mutated copy of the MECP2 gene in some cells and an active normal copy in others. Cells with the normal copy produce normal protein, which gives the girls some of the protein that they need. Alternatively, boys only have one copy of the X chromosome, and it is always active. This means that if a boy has a MECP2 mutation, he doesn't have a second normal copy of the gene the way that girls do. The result is that boys are more likely to have severe disease. In fact, most boys who are born with MECP2 mutations have severe problems and die shortly after birth. That said, a very small number of boys have classic RTT and MECP2 mutations. These mutations may produce more mild disease in girls or boys.
It is important to note that a small number of girls have a MECP2 mutation, but the chromosome with the mutation is inactive in most of their cells. These girls are clinically normal. However, they have a 50% chance of passing the mutation to a child.
Differential Diagnosis
Angelman syndrome (AS). AS is similar to RTT in many ways. The defining problems of this condition are neurological and developmental. Similarities to to RTT include a happy disposition, frequent laughter, sleep disturbances, an awkward or ataxic gait, and scoliosis. Also, as with Rett syndrome, speech in AS is severely impaired or absent. However, unlike Rett patients, who begin to speak as infants and young toddlers and then lose this skill, people with AS never develop speech. An important difference between RTT and AS is that people with RTT regress developmentally, while people with AS do not. An important example here apart from speech is the loss of purposeful use of the hands in RTT. People with AS also do not have the habit of gazing intensely at others in the way that people with RTT do. AS affects males and females equally, a feature that may help distinguish it from RTT in a male patient.
References
- 1. Neul JL et al. (2010) Rett syndrome: revised diagnostic criteria and nomenclature. Ann Neurol 68(6):944-950. Full text on PubMed.
- 2. Downs J et al. (2009) Guidelines for management of scoliosis in Rett syndrome patients based on expert consensus and clinical evidence. Spine 34(17):E607-617. Abstract on PubMed Full text on support group website.
- 3. Acampa M & Guideri F (2006) Cardiac disease and Rett syndrome. Arch Dis Child 91(5):440-443. Full text on PubMed.
- 4. Hagberg B (2002) Clinical manifestations and stages of Rett syndrome. Ment Retard Dev Disabil Res Rev 8(2):61-65. Abstract on PubMed.
- 5. Lotan M & Hanks S (2006) Physical therapy intervention for individuals with Rett syndrome. Sci World J 6:1314-1318. Full text from publisher.
- 6. Lotan M et al. (2010) Aging in persons with Rett syndrome: an updated review. Sci World J 10:778-787. Full text from publisher.
- 7. Christen HJ & Hanefeld F (1995) Male Rett variant. Neuropediatrics 26(2):81-82. Abstract on PubMed.
- 8. Renieri A et al. (2009) Diagnostic criteria for the Zappella variant of Rett syndrome (the preserved speech variant). Brain Dev 31(3):208-216. Abstract on PubMed.
- 9. Le Guen T et al. (2011) A FOXG1 mutation in a boy with congenital variant of Rett syndrome. Neurogenetics 12(1):1-8. Abstract on PubMed.
- 10. Ellaway CJ et al. (2013) 14q12 microdeletions excluding FOXG1 give rise to a congenital variant Rett syndrome-like phenotype. Hum Mol Genet 21(5):522-527. Full text on PubMed.
- 11. Rolando S (1985) Rett syndrome: report of eight cases. Brain Dev 7(3):290-296. Abstract on PubMed.
- 12. Goutieres F & Aicardi J (1986) Atypical forms of Rett syndrome. Am J Med Genet Suppl 1:183-194. Abstract on PubMed.
- 13. Hanefeld F (1985) The clinical pattern of the Rett syndrome. Brain Dev 7(3):320-325. Abstract on PubMed.
- 14. Artuso R et al. (2009) Early-onset seizure variant of Rett syndrome: definition of the clinical diagnostic criteria. Brain Dev 32(1):17-24. Abstract on PubMed.
- 15. Amir RE et al (1999) Rett syndrome is caused by mutations in X-linked MECP2, encoding methyl-CpG-binding protein 2. Nat Genet 3:185-188. Abstract on PubMed.
- 16. Ariani F et al. (2008) FOXG1 is responsible for the congenital variant of Rett syndrome. Am J Hum Genet 83(1):89-93. Full text on PubMed.
- 17. Bahi-Buisson N et al. (2008) Key clinical features to identify girls with CDKL5 mutations. Brain 131(10):2647-2661 Full text from publisher.
- 18. Scala E et al. (2005). CDKL5/STK9 is mutated in Rett syndrome variant with infantile spasms. J Med Genet 42(2):103-107. Full text on PubMed.
- 19. Tao J et al. (2004) Mutations in the X-linked cyclin-dependent kinase-like 5 (CDKL5/STK9) gene are associated with severe neurodevelopmental retardation. Am J Hum Genet 75(6):1149-1154. Full text on PubMed.
- 20. Neul JL et al. (2008) Specific mutations in methyl-CpG-binding protein 2 confer different severity in Rett syndrome. Neurology 70(16):1313-1321. Full text on PubMed.
- 21. De Bona C et al. (2000). Preserved speech variant is allelic of classic Rett syndrome. Eur J Hum Genet 8(5):325-330. Full text from publisher.
- 22. Jacob FD et al. (2009) Atypical Rett syndrome with selective FOXG1 deletion detected by comparative genomic hybridization: case report and review of literature. Eur J Hum Genet 17(12):1577-1581. Full text on PubMed.
- 23. Soultanis KC et al. (2007) Rare causes of scoliosis and spine deformity: experience and particular features. Scoliosis 2:15. doi:10.1186/1748-7161-2-15 Abstract on PubMed.
- 24. Chapleau CA et al. (2013). Rett Syndrome: a model of genetic neurodevelopmental disorders. In: Genetic Disorders Maria Puiu (Ed.), Intech ISBN: 978-953-51-0886-3 Full text.