Rubinstein-Taybi syndrome (RTS)
Clinical information
Rubinstein-Taybi syndrome is a very rare genetic condition. One study in the Netherlands estimated that it affects 1 in 100,000 to 1 in 125,000 newborns in that country (1). A very large study of 571 RTS patients diagnosed between 1957 and 1998 found that the vast majority were white: patients came from 40 countries; 14 were black, 25 were Asian (Japan and China), and the rest were Caucasian (2). In the process of gathering information for our diagnosis tool, we found reports of RTS in India (5-7; list not conclusive). No one knows if this preponderance of Caucasians is due to biological differences in European people, underdiagnosis in other groups, other factors, or a mixture of all of these factors. Facial features in RTS patients of African origin may not be similar to those of Caucasian patients, and the disease may be less obvious in this group (2). Medical problems and traits in RTS include the following:
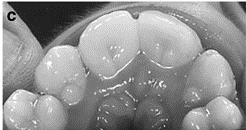
- Squared or very wide thumbs (see photos below)
- Squared or very wide big toes (see photos below)
- Squared or very wide fingers and toes see photos below)
- Intellectual disability (moderate to severe in many cases)
- Microcephaly (small head)
- Short stature (height)
- Hairiness
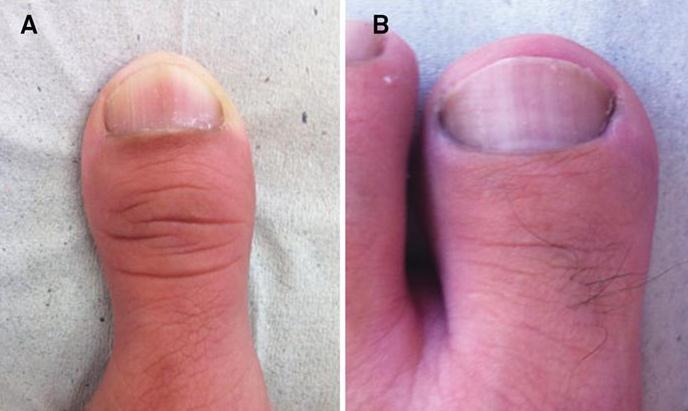
- Dental abnormalities
- Cardiac abnormalities (in up to ~40% of patients)
- Keloid scars (thick, raised scars)
- Frequent respiratory infections
Common medical problems in RTS
Size at birth is usually normal in people with RTS. Growth begins to falter soon afterward, however, and adults with this syndrome tend to be short or very short. In addition, RTS patients may have a lot of hair. They may also have eye problems including cataracts and glaucoma, although these problems occur in less than 15% of patients.
- Wide-set eyes (see photo at right)
- Highly-arched eyebrows (see photos at right)
- Downslanting palpebral fissures (the eyelids slope downward)
- Broad nasal bridge
- A grimacing smile
- Nasal septum below alae (the center tissue goes below the nostril edges; see photo on right)
- Retrognathia
- Epicanthal folds on eyes
- Malocclusion of teeth (crooked teeth)
- Talon cusps on the teeth (see photo below)
Common facial features in RTS
Although RTS patients are said to typically have moderate to severe intellectual disabilities, mild forms of the disease with mild or no intellectual disabilities have been reported (3,8). Thus, the absence of moderate to severe mental retardation does not preclude a diagnosis of RTS. NIH's OMIM entry on what is called Type 1 RTS OMIM has a brief discussion of this topic. Many mild cases of RTS appear to be caused by mutations in a gene called EP300. OMIM also has entry on EP300 RTS.
RTS is usually diagnosed clinically, although confirmation via molecular methods can make a definitive diagnosis. RTS results from mutations in either of two genes: CREBBP or EP300. The mutations appear to arise spontaneously, and most people with RTS are the only people in their family with the syndrome. However, one parent may occasionally have a mild form of the disease (3,4). The risk that siblings will be affected is apparently <1%. If you or your child's doctor suspects RTS, a sample can be sent to a testing center (see information in link at right).
The University Hospital Bordeaux (France) conducted a small study of the effects of sodium valproate in RTS. Sodium valproate is used to treat seizures. The goals of the study were to see if this drug could improve learning and memory and fine motor skills in people with RTS. In addition to evaluating outcomes with clinical tests such as memory and motor skill testing, the study leaders used brain imaging and specialized testing. The trial was completed in March, 2015. More information about the study, including contact information, is available at clinicaltrials.gov.
The broad thumbs, fingers, and toes that occur in RTS also occur in other diseases, most noably the FGFR-related craniosynostosis syndromes, such as Pfeiffer syndrome, Apert syndrome, Crouzon syndrome, Beare-Stevenson syndrome, and a number of other similar conditions. The term craniosynostosis refers to an abnormality in which the bones in an infant's skull fuse prematurely. At birth, these bones are are connected by soft tissue that lets the skull expand as the infant's brain grows. When the bones fuse prematurely, the soft tissue is gone, and the skull cannot grow properly. Craniosynostosis does notv appear to occur in RTS, and its presence indicates that RTS may not be the correct diagnosis.
Keipert syndrome (KS) is another condition that causes broad thumbs and toes. Keipert syndrome is also known by the name nasodigitoacoustic syndrome. Some of the medical problems associated with KS overlap with RTS. They include deafness, which occurs in a minority of RTS patients, and wideset eyes. One feature that may distinguish KS from RTS is that intelligence is usually normal or only mildly impaired in KS, whereas it intellectual disability in RTS is generally moderate to severe (IQs are typically 35 to 60 although they are not always in this range; 9). KS patients also have very short fingers.
KS is caused by mutations in a gene on the X chromosome (Xq22.2-q28), meaning that it is typically passed from a mother to her son. Females do not usually show signs of KS, although one female patient has been reported; this patiet is thought to have inherited KS from her father as an autosomal dominant disorder (10). However, and generally speaking, KS appears to be an unlikely diagnosis in a female. Genetic testing for RTS can help distinguish the two conditions.
References
- 1. Hennekam RC et al. (1990) Rubinstein-Taybi syndrome in the Netherlands. Am J Med Genet Suppl 6:17-29. Abstract on PubMed.
- 2. Rubinstein JH (1990) Broad Thumb-Hallux (Rubinstein-Taybi) Syndrome 1957-1988. Am J Med Genet Suppl 6:3-16. Abstract on PubMed.
- 3. Bartsch O et al. (2010) Two patients with EP300 mutations and facial dysmorphism different from the classic Rubinstein-Taybi syndrome. Am J Med Genet A 152A:181-184. Abstract on PubMed.
- 4. Chiang PW et al. (2009) Somatic and germ-line mosaicism in Rubinstein-Taybi syndrome. Am J Med Genet A 149A(7):1463-1467. Abstract on PubMed.
- 5. Darlong V et al. (2014) Perioperative management of a patient of Rubinstein-Taybi syndrome with ovarian cyst for laparotomy. Journal of Anaesthesiology Clinical Pharmacology 30(3):422-424. Full text on PubMed.
- 6. Bansal S et al. (2013) Rubinstein-Taybi syndrome: A report of two siblings with unreported cutaneous stigmata. Indian J Dermatol Venereol Leprol 79(5):714-717. Full text from publisher.
- 7. Kumar S et al. (2012) Rubinstein-taybi syndrome: Clinical profile of 11 patients and review of literature. Indian J Hum Genet 18(2):161-166. Full text on PubMed.
- 8. Bartsch O et al. (2002) Molecular studies in 10 cases of Rubinstein-Taybi syndrome, including a mild variant showing a missense mutation in codon 1175 of CREBBP. Med Genet 39:496-501. Full text on PubMed.
- 9. Hennekam RC et al. (2006) Rubinstein-Taybi syndrome. Eur J Hum Genet 14:981-985. Full text from publisher.
- 10. Dumic RC et al. (2006) Rubinstein-Taybi syndrome. Am J Med Genet A 140(22):2488-2492. Abstract on PubMed.
- 11. Bentivegna A et al. (2006) Rubinstein-Taybi Syndrome: spectrum of CREBBP mutations in Italian patients. BMC Med Genet 7:77. Full text on PubMed.
- 12. Silva CC et al. (2014) Broad thumbs and broad hallux: the hallmarks for the Rubinstein-Taybi syndrome. Arq Neuro-Psiquiatr 72(1):81-82. Full text from Scielo.
- 13. Tirali A et al. (2014) Oro-facio-dental findings of Rubinstein-Taybi syndrome as a useful diagnostic feature. J Clin Diag Res 8(1): 276-278. Full text on PubMed.
- 14. Da Oger G (2011) Cicatrices chéloïdes sur torse et bras, après plaies superficielles il y a environ 6 mois (Keloid scars on the chest and arms, roughly 6 months after superficial injuries occurred). Photo on Wikimedia Commons.