Saethre-Chotzen Syndrome (SCS)
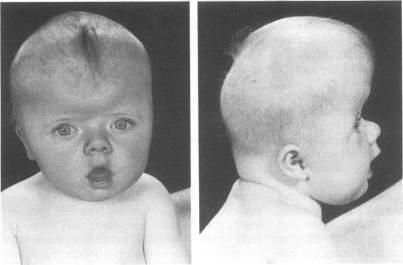
Saethre-Chotzen syndrome (SCS) is member of a group of disorders involving craniosynostosis. This term means that at least one of a person's skull bones fuses prematurely. The problem is often noted at birth, but it may be picked up on an ultrasound or it may not become evident until well after birth. Premature fusion of skull bones restricts skull growth, causing it to expand unevenly to accomodate brain growth.
When only one brain suture is closed prematurely, a person is said to have isolated craniosynostosis. This condition is relatively common, occuring in roughly 3-5 per 10,000 births or even more frequently (1, 2). Severity varies widely, with some cases being severe and others being barely noticeable. The causes for isolated craniosynostosis are not fully understood, but hereditary/genetic components are involved (1, 3). Possible risk factors for craniosynostosis include, but are not limited to, the mother's age and race (more common among older women and whites; 4), male sex (4), and heavy maternal smoking, especially after the first trimester (5).
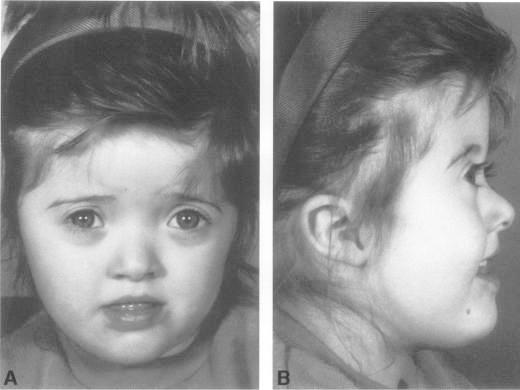
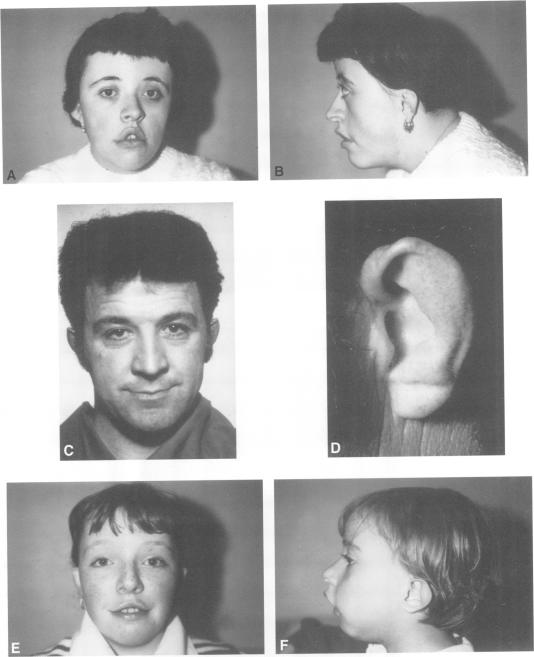
In addition to isolated craniosynostosis, there are also a number of craniosynostosis syndromes. As the name implies, the syndromic forms of craniosynostosis involve problems in a variety of body systems. The hands and/or feet are often affected, a fact that implies that skull and hand/foot development share some type of common mechanism. Saethre-Chotzen syndrome is a craniosynostosis syndrome caused by mutations in the gene TWIST1. Other craniosynostosis syndromes are caused by mutations in the genes FGFR1, FGFR2, or FGFR3. This group includes Crouzon syndrome, Crouzon syndrome with acanthosis nigricans, Pfeiffer syndrome, Apert syndrome, Muenke syndrome, Jackson-Weiss syndrome, Beare-Stevenson syndrome, and FGFR2-related isolated coronal synostosis (6, 7). Generally speaking, skull abnormalities in these syndromes are observed in the newborn period or before, although some cases may not be noted until later infancy or afterward. In addition to having abnormally shaped skulls, people with these syndromes tend to have wideset eyes that protrude outward (proptosis), an underdeveloped midface (hypoplasia; best seen in profile; see photos on this page), a small nose that may be beaked, and a highly arched palate or a cleft palate (see photos accompanying Crouzon syndrome). Intellectual disability is common but does not always occur (6-8).
Saethre-Chotzen syndrome affects males and females equally. In our analysis of SCS patients, 46% were male and 54% were female. SCS has also been seen in many races and ethnic groups around the world.
Estimates about the prevalence of Saethre-Chotzen syndrome vary. The current estimate one per 25,000 to 50,000 births (6, 8). The variability in the clinical features of those affected suggests that the current estimates may be somewhat low (8, 9).
Saethre-Chotzen syndrome is also called type III acrocephalosyndactyly (8).
Clinical information
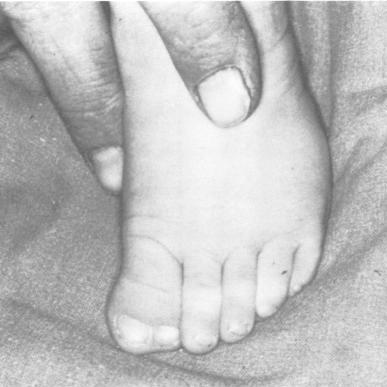
The cardinal features of SCS are craniosynostosis, (typically involving coronal sutures), facial asymmetry, and abnormalities of the ear and/or hallux (large toe). Midface hypoplasia is also very common in SCS. This term means that a portion of the middle part of the face is underdeveloped. When viewed in profile, people with midface hypoplasia often appear to have a flat or convex facial structure (see photos on this page). Tear duct abnormalities are common in SCS. A highly arched palate is also common; cleft lip or palate occurs in a minority of cases (8, 9).
Most people with Saethre-Chotzen syndrome do not have an intellectual disability. However, intellectual disability should not be used to exclude a diagnosis of SCS, as craniosynostosis can cause elevated pressure in the brain (6, 10). This problem can cause intellectual disability to develop over time (6-9). More commonly, language delays in childhood occura and result from hearing loss, which may be related to nerve compression caused by high intracranial pressure (9-11).
Many persons with CSC have such subtle clinical features, and the syndrome is not diagnosed until a family member or child is diagnosed (6, 8, 9).
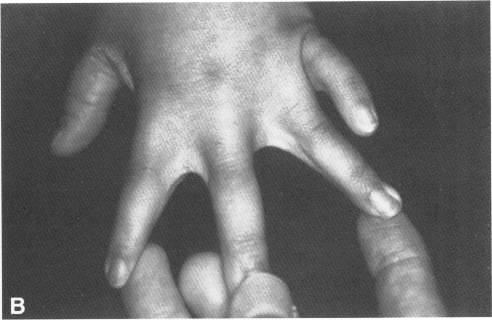
Usually syndactyly in SCS involves the first two fingers of the hands or the second and third toes, and is cutaneous (only involves the soft tissues). Mild cutaneous syndactyly may resemble webbing between involved digits. (See photos this page; 6, 8).
The following are common clinical features of Saethre-Chotzen syndrome. Because SCS symptoms overlap with several other craniosynostosis syndromes, laboratory testing may be required to make a definitive diagnosis.
- Craniosynostosis (premature fusion of the skull bones, accompanied by unusual skull shape
- Abnormalities of the external parts of the ear (see photos on this page)
- Dental abnormalities (crowding, abnormally positioned teeth, etc.)
- Deformities of the hallux (big toe); large or squared terminus
- Syndactyly of the hands and feet (may resemble webbing)
- Enlargement of the brain ventricles (on scan)
- Tear duct abnormalities
- Highly arched palate
- Hearing problems
Common clinical features of Saethre-Chotzen syndrome
In addition, people with SCS often share a similar facial appearance and may have the following facial features. Note that many of these features are shared with members of the FGFR-related craniosynostosis syndromes, including Crouzon, Apert, Muenke, and Pfeiffer syndromes:
- Midface hypoplasia (underdevelopment of cheekbones, upper jaw, and eye sockets)
- Downslanting palpebral fissures (see photos this page)
- Proptosis/protruding eyes (usually mild in CSC)
- Ptosis (drooping of upper eyelids)
- Hypertelorism/wideset eyes
- Strabismus/unaligned eyes
- Low-set or rotated ears
- Deviated nasalseptum
- Facial assymetry
- Large forehead
Early diagnosis benefits patients because they can be monitored carefully and cared for during childhood so as to avoid some of the consequences of vision or hearing difficulties and increased intracranial pressure. Surgeries to reshape the skull are common (6-10), as is surgical correction of severe ptosis or strabismus (8). Dental abnormalities are also a very common problem in SCS, and may require treatment (8).
Note that Robinow-Sorauf syndrome is caused by mutations in TWIST1. Although once considered to be a distinct condition, it is now considered to be a form of SCS (8). It is characterized by SCS features paired with duplicated big toes and bunions.
Diagnosis and Testing
SCS should generally be suspected in an infant or older person who presents with craniosynostosis, ptosis, cutaneous syndactyly (of toes or fingers) and unusual ear morphology that includes a prominent crus helix. These abnormalities occur commonly in people with SCS.
SCS is generally caused by mutations in the gene TWIST1, but it is also associated with FGFR2 (12). It is an autosomal dominant disorder. This term means that it is usually passed from one affected parent to a child. SCS may also occur sporadically when a gene mutation arises spontaneously. (6, 8).
The link at the upper right part of this page provides information about laboratories and other facilities that perform testing for SCS. There is also a link for generalized testing for craniosynostoses.
Differential Diagnosis
The differential diagnosis for SCS includes several other craniosynostosis syndromes.
Muenke syndrome. Muenke syndrome and SCS share many clinical features, including similar patterns of craniosynostosis. However, persons with SCS typically have distinguishing features such as ptosis that may worsen with time, low hairline at the forehead, and specific deformities of the large toes. However, people with Muenke syndrome do not have the facial features that are common to SCS (low hairline, downslanting palpebral fissures, droopy eyelids/ptosis), nor do the have webbing of the fingers or toes or abnormalities of ear anatomy (8). People with Muenke syndrome are more likely to have hearing loss and mental disability (10). SCS is more likely to result in early and severe high intracranial pressure, however (8, 10). Muenke syndrome is caused by mutation in the gene FGFR3, whereas SCS is associated mutations in TWIST1 and FGFR2 (12). This fact means that genetic testing should distinguish the two syndromes (8).
Baller-Gerold syndrome (BGS). BGS is a craniosynostosis syndrome. Like SCS, the coronal sutures are usually involved, though other sutures may also be affected. Patients with both conditions may have bulging eyes and flat skulls. However, unlike SCS patients, BGS patients may have fewer than 10 fingers or toes. They may also have elbow, lower arm and hand malformations, which are unusual in SCS. BGS usually causes intellectual disability, which is unusual in SCS but does occur. BGS is caused by mutations in the gene RECQL4 and is inherited in an autosomal recessive manner, which means that both parents must pass on a copy of a mutated gene (6).
Apert syndrome (AS). AS is similar to SCS. People with both conditions have craniosynostosis, wideset eyes, proptosis/protruding eyes, and dental abnormalities (13). Unlike Apert syndrome, however, Saetreh-Chotzen syndrome does not cause severe syndactyly of the the hands and feet (at least three fingers and/or toes fused; often all five). Given that syndacytly is universal and severe in AS, its presence or absence can help distinguish the two conditions. In addition, most patients with Apert syndrome have intellectual disabilities (13) while a majority of SCS patients do not (8).
Crouzon syndrome (CS). Crouzon syndrome is the most common of the craniosynostosis syndromes, and is also very similar to CSC. People with both syndromes have craniosynostosis, wideset eyes, and dental abnormalities. Proptosis is nearly universal in CS, and is much more pronounced than in most cases of SCS. As in SCS, intellectual disability is uncommon. Unlike SCS, however, Crouzon syndrome does not generally affect the external parts of the ears, nor the hands and feet. Hearing problems are also unusual in CS, and they are more common in SCS (6-8).
Pfeiffer syndrome (PS). Pfeiffer syndrome is another craniosynostosis syndrome. It is also similar to SCS. People with PS have craniosynostosis, foot syndactyly, proptosis/protruding eyes, highly arched palates and dental abnormalities. They may also have facial asymmetry and downslanting palpebral fissures. Intellectual disability occurs in PS, but intelligence is normal in the majority of patients. Unlike SCS syndrome, however, PS does not generally cause syndactyly of the hands. This clinical feature can help distinguish the two conditions (6, 7).
Jackson-Weiss syndrome (JWS). JWS is a very rare member of FGFR-related craniosynostosis syndromes group. It was reported in a large Amish kindred in 1976 and is similar to AS (14). As with SCS, people with JWS have craniosynostosis, wideset eyes, and foot abnormalities. Unlike Saethre-Chotzen syndrome, however, JWS does not generally cause syndacytly of the hands. Given that this abnormality may occur in SCS, its presence can help distinguish the two conditions. Relatively few studies have reported on JWS; the largest did not find evidence of intellectual disability, although it has been reported in a smaller study (15).
SCS is an autosomal dominant disorder, and most people with SCS have an affected parent, though it may not be clear that a nearly-asymptomatic parent has passed the syndrome to a child (8). Family photographs may be helpful in establishing inheritance, as the clinical features of SCS vary, even in affected members in the same family. Severity ranges from asymptomatic to severe.
Because Saethre-Chotzen syndrome has also been found in people with FGFR2 mutations, TWIST1 and FGFR testing for suspected Saethre-Chotzen syndrome should also include analysis of FGFR2, FGFR3, as well as TWIST1 (6, 8, 12, 16).
References
- 1. Cohen MM & MacLean RE, eds. (2000) Craniosynostosis: Diagnosis, evaluation, and management. New York: Oxford University Press.
- 2. Reefhuis J et al. (2003) Fertility treatments and craniosynostosis: California, Georgia, and Iowa, 1993-2021. Pediatrics 111(5 Pt 2):1163-1166. Full text from publisher.
- 3. Boyadjiev SA et al. (2007) Genetic analysis of non-syndromic craniosynostosis. Orthod Craniofac Res 10(3):129-137. Abstract on PubMed.
- 4. Alderman BW et al. (1988) An epidemiologic study of craniosynostosis: risk indicators for the occurrence of craniosynostosis in Colorado. Am J Epidemiol 128:431-433. Abstract on PubMed.
- 5. Carmichael SL et al. (2008) Craniosynostosis and maternal smoking. Birth Defects Res A Clin Mol Teratol 82(2):78-85. Abstract on PubMed.
- 6. Robin NH et al. (1998) FGFR-Related Craniosynostosis Syndromes. Updated June 7, 2011. GeneReviews [Internet] Pagon RA et al., editors. Seattle (WA): University of Washington, Seattle; 1993-2018. Full text.
- 7. Wilkie AO (1997) Craniosynostosis: genes and mechanisms. Hum Mol Genet 6(10):1647-1656. Abstract on PubMed.
- 8. Gallagher ER et al. (2003) Saethre-Chotzen Syndrome. Updated June 14 2012 GeneReviews [Internet] Pagon RA et al. editors. Seattle (WA): University of Washington, Seattle; 1993-2018. Full text.
- 9. Reardon W & Winter RM (1994). Saethre-Chotzen syndrome. J Med Genet 31(5):393-396. Full text on PubMed.
- 10. Kress W et al. (2006) Saethre-Chotzen syndrome caused by TWIST 1 gene mutations: functional differentiation from Muenke coronal synostosis syndrome. Eur J Hum Genet 14(1):39-48. Full text from publisher.
- 11. Arduino-Meirelles AP et al. (2006) Developmental aspects of oral language in craniosynostosis. Pró-Fono Revista de Atualizaçâo Científica 18(2):213-220. Full text from Scielo.
- 12. Paznekas WA et al. (1998) Genetic heterogeneity of Saethre-Chotzen syndrome, due to TWIST and FGFR mutations. Am J Hum Genet 62(6):1370-1380. Full text on PubMed.
- 13. Renier D et al. (1996) Prognosis for mental function in Apert's syndrome. J Neurosurg 85(1):66-72. Abstract on PubMed. Full text on ResearchGate.
- 14. Jackson CE et al. (1976) Craniosynostosis, midfacial hypoplasia and foot abnormalities: an autosomal dominant phenotype in a large Amish kindred. J Pediatr 88(6):963-968. Abstract on PubMed.
- 15. Cross HE et al. (1969) Craniosynostosis in the Amish. J Pediatr 75:1037-1044. Abstract on publisher website.
- 16. Freitas EC et al. (2006) Q289P mutation in FGFR2 gene causes Saethre-Chotzen syndrome: some considerations about familial heterogeneity. Cleft Palate Craniofac J 43(2):142-147. Abstract on PubMed.
- 17. Wilkie AO et al. (1995) Saethre-Chotzen syndrome associated with balanced translocations involving 7p21: three further families. J Med Genet 32(3): 174-180. Full text on PubMed.
- 18. Carter CO et al. (1982). A family study of craniosynostosis, with probable recognition of a distinct syndrome. J Med Genet 19(4): 280-285. Full text on PubMed.
- 19. National Human Genome Research Institute. Elements of Morphology: Human Malformation Terminology (Online encyclopedia).